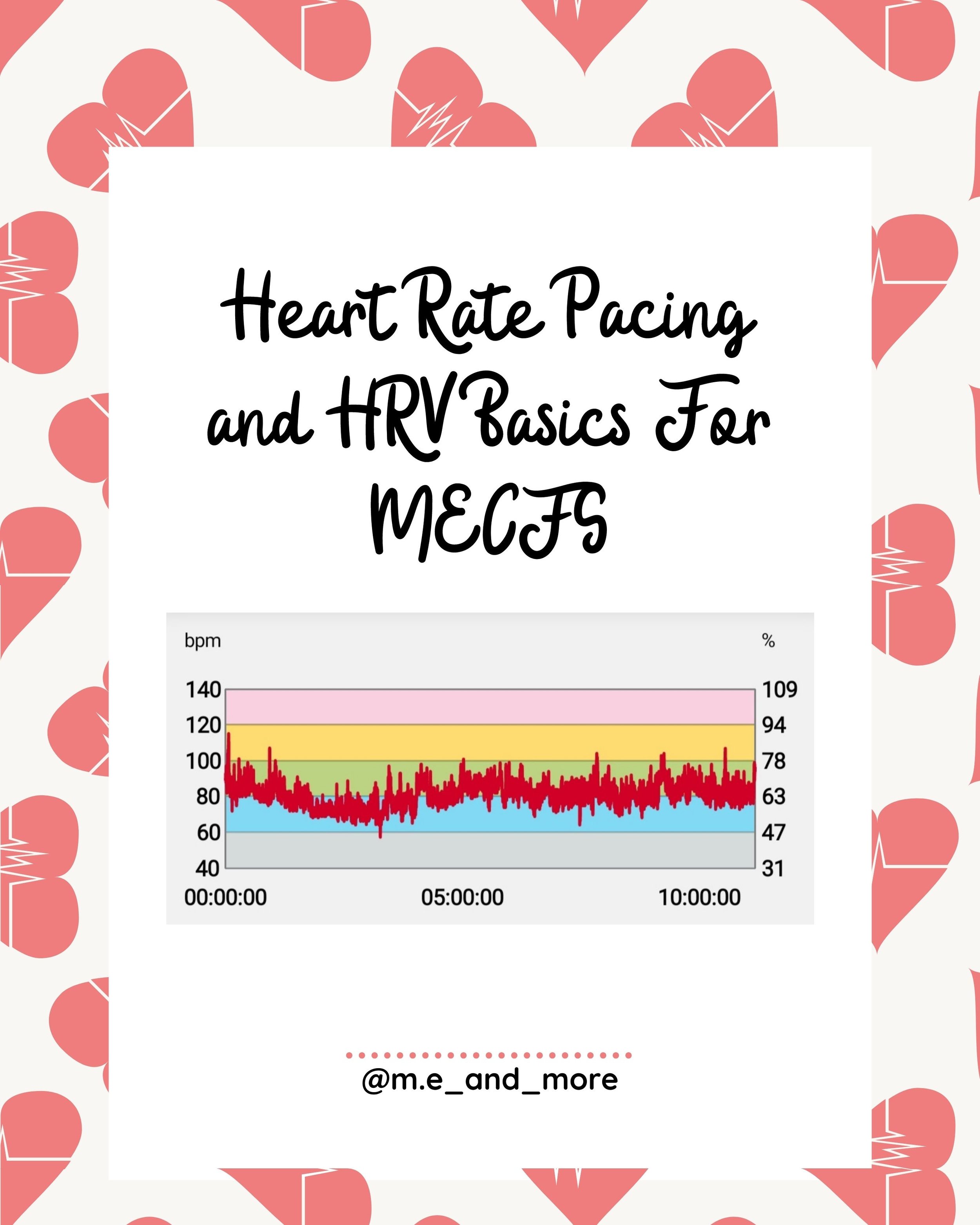
Heart Rate Pacing and HRV… Basics For MECFS
Disclaimer:
Heart rate pacing is a very aggressive form of pacing that is only suitable to patients with myalgic encephalomyelitis aka MECFS who suffer from post-exertional malaise.
Post-exertional malaise is an exacerbation of numerous illness symptoms 24-48 hours after exertion.
Patients with MECFS should see their morning resting hr decrease following the implementation of hr pacing. This is the opposite response to non-MECFS patients who would expect to see heart rate rise from deconditioning.
Conditions that do not benefit from hr pacing include: EDS, Fibromyalgia, MS, POTS, and most autoimmune disease.
Patients with both MECFS and these other conditions should carefully monitor their response to heart rate pacing and discontinue if it increases their symptoms.
-----
What Is Heart Rate Pacing?
Heart rate pacing is the practice of using a heart rate monitor such as a watch, armband, or chest strap to monitor heart rate and keep your heart rate under a given threshold.
Heart rate pacing allows for an objective measure of when you are overexerting. This can help patients, especially those new to MECFS to better learn where their limits are and prevent PEM. It can also help patients who do not experience many symptoms during exertion but experience severe PEM.
------
What Is HRV?
Heart rate variability is a measurement of how responsive your heart rate is, in other words, how much it varies between beats. For MECFS patients HRV is a good indicator of sympathetic and parasympathetic nervous system balance.
High HRV = Parasympathetic Dominance
This is your body's rest and digest mode. In general, this state is desirable for persons with ME.
Low HRV = Sympathetic Dominance
This is your body's fight or flight mode. If your HRV is very low you may be in a crash or experiencing an adrenaline surge (wired but tired).
Because of how HRV is calculated, it is closely linked with resting hr. When your resting hr is lower your HRV is normally higher. When your resting hr is higher your HRV is normally lower.
----
Anatomy Of A Crash:
It is important to understand the different stages of a crash in order to effectively pace through it. These are as follows:
1.) Post exertion low: Immediately following your exertion your hr increases and your hrv decreases.
2.) Parasympathetic swing:
Next, you will have an extremely high HRV indicating an active parasympathetic nervous system. I feel better during this time and get a lot of sleep.
3.) Big crash:
Swinging the other way you will then get a very low HRV as your sympathetic nervous system takes over. You might feel "wired but tired" at this point.
4.) Stabilization
Over the next few days, you will continue to swing between high and low until you stabilize around a baseline number. When your readings are mostly constant you are likely just about done crashing.
The next slides will talk about how you can use different pacing tools to know where in this cycle you are and respond accordingly.
----
HR Pacing Tool #1: Morning Resting HR
The simplest form of hr pacing you can implement is to start taking your resting hr each morning when you wake up. It is important to do this at a consistent time each day. Alternatively, you can get this measurement from a device that takes your resting hr during your sleep.
If your morning resting hr is 10-15bpm higher than normal This likely indicates a crash. You should minimize all activity for the day and cancel any big plans.
If your morning resting hr is low this may indicate recovery out of a crash for those new to hr pacing or may indicate a parasympathetic swing if you have recently overexerted.
-----
HR Pacing Tool #2: Threshold Alarm
This tool involves setting an alarm at your anaerobic threshold or the point at which you begin to trigger PEM. The anaerobic threshold is the point at which your body stops using oxygen to generate ATP and instead uses a process that generates lactic acid. In people with ME the point at which this transition takes place is much lower.
The only true way to determine your anaerobic threshold is a 2-day CPET (it will be lower when you are in PEM on day 2) However, this can be dangerous or unfeasible for moderate to severe patients.
The most common way to determine the threshold is to pick a conservative starting number, ensure that you are not experiencing PEM and then slowly increase your threshold until you find the point at which you trigger PEM (at which point you will stay there unless you start to feel more energized)
Workwell foundation advises a starting threshold of 15bpm above your resting hr. However, this is often too low for many people to even attempt. A common formula is
(220 - age) × (severity multiplier)
Which can be adjusted based on how severe your ME is to somewhere between 0.5 and 0.75
Another common choice is simply to start at 100bpm.
----
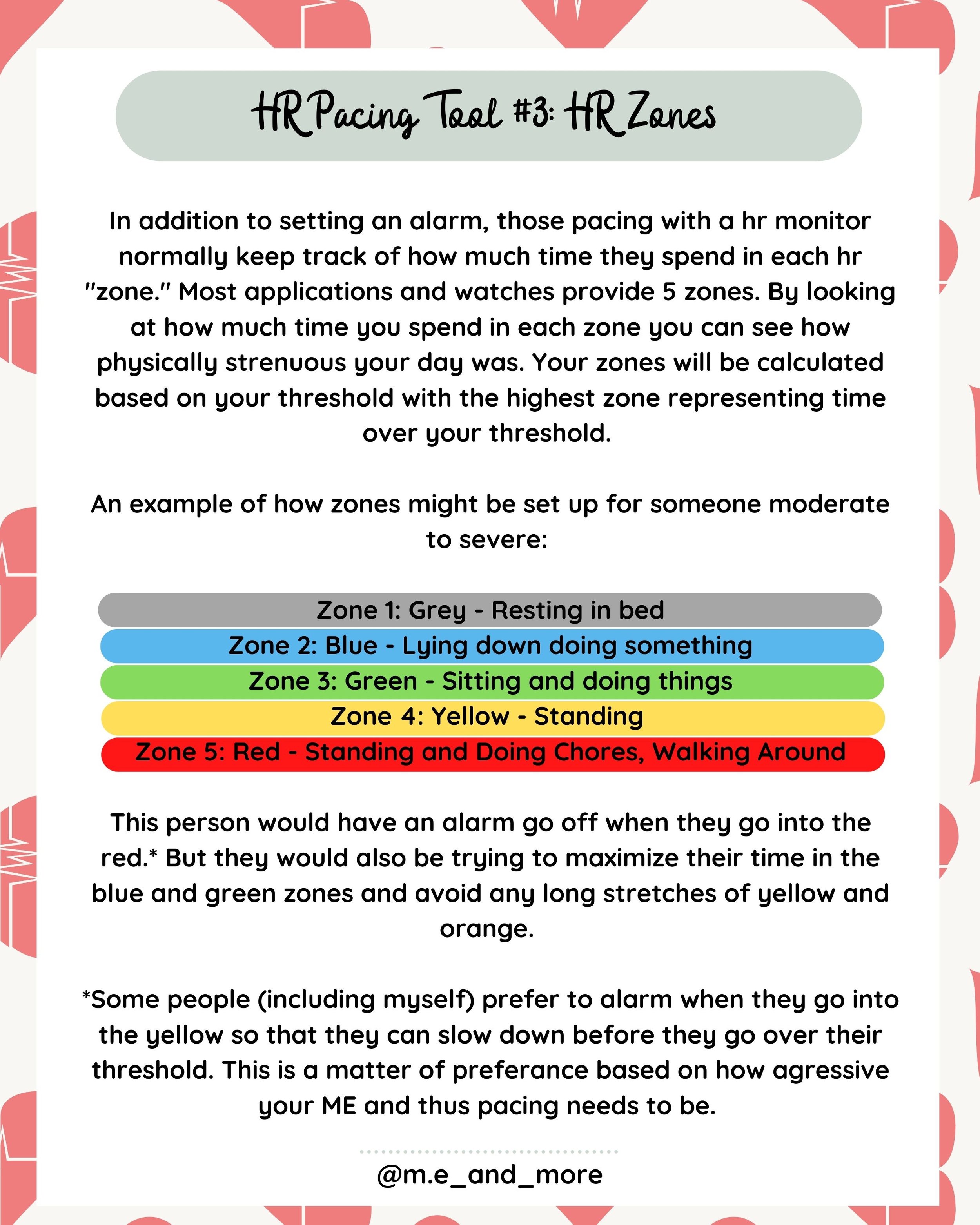
HR Pacing Tool #3: HR Zones
In addition to setting an alarm, those pacing with a heart rate monitor normally keep track of how much time they spend in each hr "zone." Most applications and watches provide 5 zones. By looking at how much time you spend in each zone you can see how physically strenuous your day was. Your zones will be calculated based on your threshold with the highest zone representing time over your threshold.
An example of how zones might be set up for someone moderate to severe:
Zone 1: Grey - Resting in bed
Zone 2: Blue - Lying down doing something
Zone 3: Green - Sitting and doing things
Zone 4: Yellow - Standing
Zone 5: Red - Standing and Doing Chores, Walking Around
This person would have an alarm go off when they go into the red.* But they would also be trying to maximize their time in the blue and green zones and avoid any long stretches of yellow and orange.
*Some people (including myself) prefer to alarm when they go into the yellow so that they can slow down before they go over their threshold. This is a matter of preference based on how aggressive your ME and thus pacing needs to be.
-----
HR Pacing Tool #4: HRV Monitoring
HRV monitoring allows you to get a gauge for your parasympathetic vs sympathetic balance through brief 5+ minutes readings.
The most important HRV reading is your morning measurement. Like your resting hr this should be taken when you wake up and gives you an idea of your baseline for the day. Note that some apps like Elite HRV will give you a readiness score for the day based on your own personal numbers while others will use non-personalized data.
Some valuable ways of interpreting this data include:
Low HRV indicates sympathetic dominance
High HRV indicates parasympathetic dominance
High variability of HRV between different days indicates a crash or rolling crash
A sharp drop in HRV after an activity indicates potential overexertion
Stable HRV or slowly rising HRV indicates good pacing or recovery
Note: HRV is a highly sensitive measurement. If you want to use HRV to help you make decisions about pacing it is highly recommended that you purchase a reliable chest strap like the Polar H10. Watches and other monitors may offer HRV functionality but the quality of this data is very questionable.
-----
Practical Implementation:
There is far more to the practical implementation of hr pacing than I can cover here. Thankfully, amazing resources already exist. As such I will only provide a brief overview of the most popular apps and devices. For detailed comparison, I highly recommend reading the guidance resources and joining the Facebook groups before purchasing anything.
Devices:
Polar H10 Chest Strap (best HRV)
Polar M430 Watch
Garmin Vivosmart
Apple Watch
Apps:
EliteHRV
Pulsometer
Heart Graph
Welltory
HRV4Training
Guidance:
Workwell Foundation HR Pacing Guidelines
Angela Flack's Guide To HR Pacing
Facebook Groups:
MECFS: Below The Threshold
HR Pacing for MECFS: Discussion
----
Heart Rate Pacing is a powerful tool for patients with Myalgic Encephalomyelitis aka MECFS to control PEM / PENE using objective heart rate and heart rate variability data.
Post-exertional malaise is the distinguishing symptom of ME / CFS and refers to an exacerbation of symptoms 24-48 hours after exertion. It causes metabolic dysfunction similar and in many ways identical to over training Syndrome in athletes. For this reason, HRV and heart rate monitors and apps used by athletes to detect and prevent overtraining syndrome by monitoring for autonomic Dysfunction can be used to detect and prevent PEM.
When you are going into PEM
-Resting hr increases
-HRV decreases (or swings between extremes)
-POTS & Tachycardia is more easily triggered
-HR responds unpredictably to exertion
When you are at baseline or in recovery
-Resting hr decreases
-HRV increases and stabilizes
-POTS & Tachycardia are less triggered
-HR responds predictably to exertion
Tracking these markers can be crucial to making decisions about how to Stop Rest Pace effectively. Remember, pacing is different for persons with ME. We do not just need to stop when we feel fatigue we need to stop before we trigger PEM. This will not always come with a lot of immediate symptoms as PEM happens primarily in the days following exertion. HR Pacing can help you know when to stop before you feel it and over time learn where your boundaries are.
It is important to note that in ME patients the following is expected upon implementing aggressive Pacing:
-Decreased resting hr
-Increased HRV
If the opposite occurs this is either an indication that you do not have MECFS (investigate for fibromyalgia, EDS, MCAS and other sources of chronic Fatigue) or that setting up and monitoring your hr is causing PEM (possible in bedbound patients with significant mental PEM)
This post is only a brief introduction. If you wish to start hr pacing I highly recommend following Angela Flacks comprehensive guide and joining the Facebook groups for guidance. Her contributions to the MECFS Community are invaluable.